Resistance is Futile
Celia Schiffer
University of Massachusetts Medical School
Published July 28, 2017
Celia Schiffer | University of Massachusetts Medical School
Approximately 200 million people are infected with hepatitis C virus (HCV) worldwide. While novel drugs, such as protease inhibitors, are effective against the virus, resistance to them evolves rapidly.
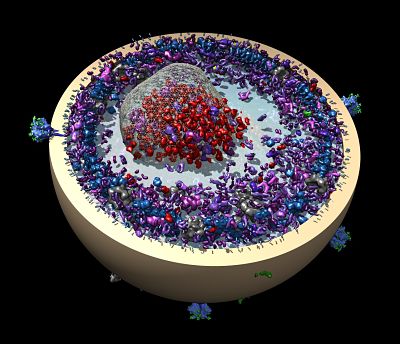
In 2016, however, Celia Schiffer, professor of biochemistry and molecular pharmacology at the University of Massachusetts Medical School, applied a smart drug development approach to the design of new HCV protease inhibitors. The strategy, which she developed a decade ago, minimizes the emergence of resistance by using structural biology and other tools to guide the design of chemicals that bind precisely to an active site on a protein.
Her experimental HCV protease inhibitors are extremely potent in in vitro laboratory tests and cut down the probability of the emergence of resistant strains of the virus substantially. “We’re not ever going to get around evolution. Drug resistance is eventually going to arise,” says Schiffer. “But we can make it tougher by being smarter about how we do drug design.”
Schiffer was originally inspired to become a scientist by her parents, for whom science was and remains a lifelong passion. In fact, Schiffer’s mother, Marianne Schiffer, is a crystallographer who invented helical wheels in 1967, though that work didn’t directly influence Schiffer, her mother’s love of science did. “I didn’t know exactly what she was doing until I was practically doing it myself,” she says.
Schiffer chose to study physics at the University of Chicago as an undergraduate because she wanted to keep her options open. At the University of California, San Francisco, she chose to study biophysics in graduate school. “I never really liked the hard distinctions between different fields in science. Biophysics was a mixture of physics, chemistry, and biology, which seemed like a good compromise,” she says.
As an undergraduate, Schiffer had used electron microscopy to study sickle cell hemoglobin. The work visualizing biologically relevant molecules intrigued her. She went on to learn crystallography and molecular modeling at UCSF. Her multidisciplinary training led her to form a multidisciplinary laboratory at the UMass Medical Center.
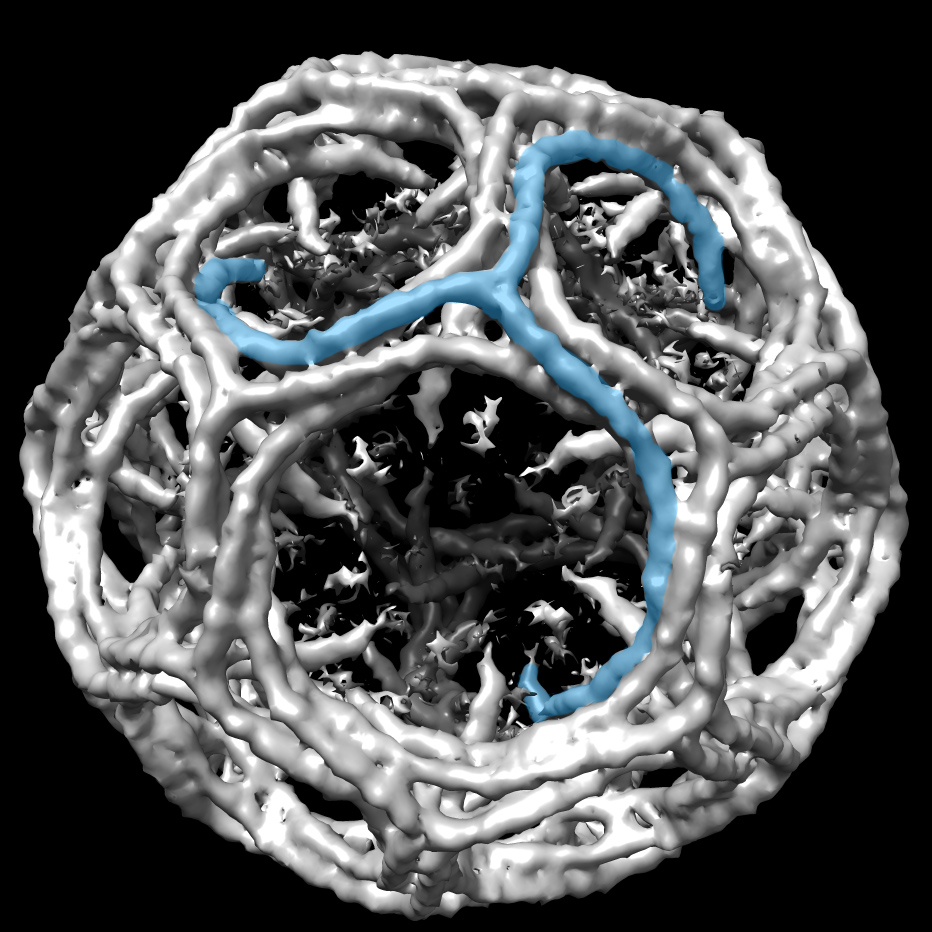
In 2003, Schiffer began studying HIV protease inhibitors to learn more about how resistance to the drugs evolves. For several years, Schiffer analyzed the patterns of resistance and found that most of the mutations that conferred resistance blocked the binding of the drug but did not interfere with the enzymatic activity of the protease. “The drugs block the scissor action of the protease, but when resistance occurs, the drug is no longer able to bind and the enzyme is still able to cut its substrates,” she says.
This observation led her to develop the concept of a substrate envelope, a tiny critical area in which the enzymatic activity occurs in the protein. By designing drugs that bind precisely within the substrate envelope, she speculated, it could be possible to minimize resistance. “Any mutation that happens within the substrate envelope will not only impact the binding of the drug but also will impact the recognition of the substrate,” she says.
In other words, resistance will block the drug, but it will also undermine the enzyme’s function. Schiffer has since published multiple papers exploring the potential for developing smarter resistance-resistant protease inhibitors to fight HIV.
In addition, she recognized that her strategy was generalizable to other fast-evolving threats. “For cancer, viruses, bacteria, or even herbicides and pesticides, there are many parallels,” she says. “We don’t have to reinvent the wheel each time.”
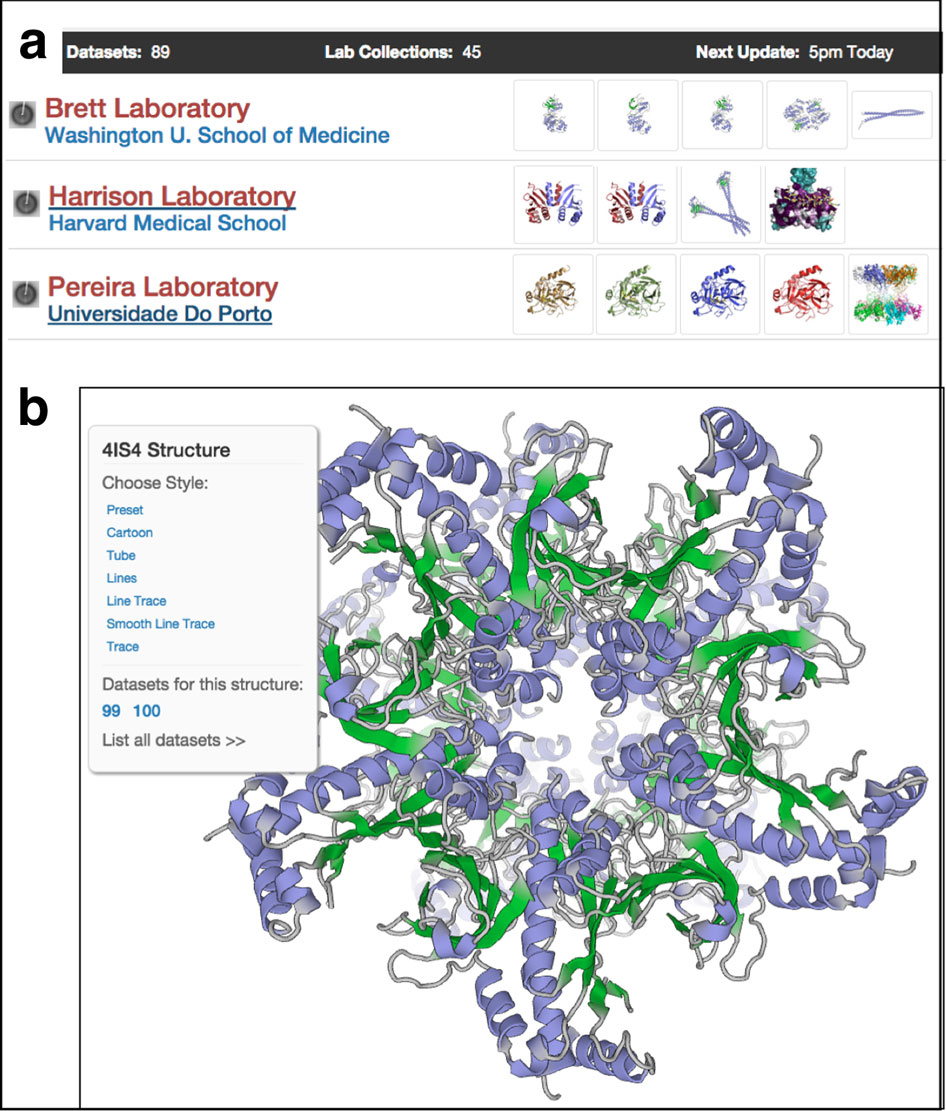
To expand the reach of this strategy and continue to develop it, Schiffer founded the Institute for Drug Resistance, a community of scientists from many backgrounds, including chemistry, virology, structural biology, and bioinformatics, all working together to understand its potential. In her lab, Schiffer has also applied the strategy to influenza, with support from the Department of Defense, and to HCV and Dengue Fever.
Further, she has begun collaborative work with Schrødinger to determine if it is possible to add new computational tools to the suite that will help guide drug design with resistance in mind early on in the design process. The work is just beginning, but Schiffer hopes that such tools would make the strategy more accessible to drug developers working inside pharmaceutical companies.
Elizabeth Dougherty